| << Chapter < Page | Chapter >> Page > |
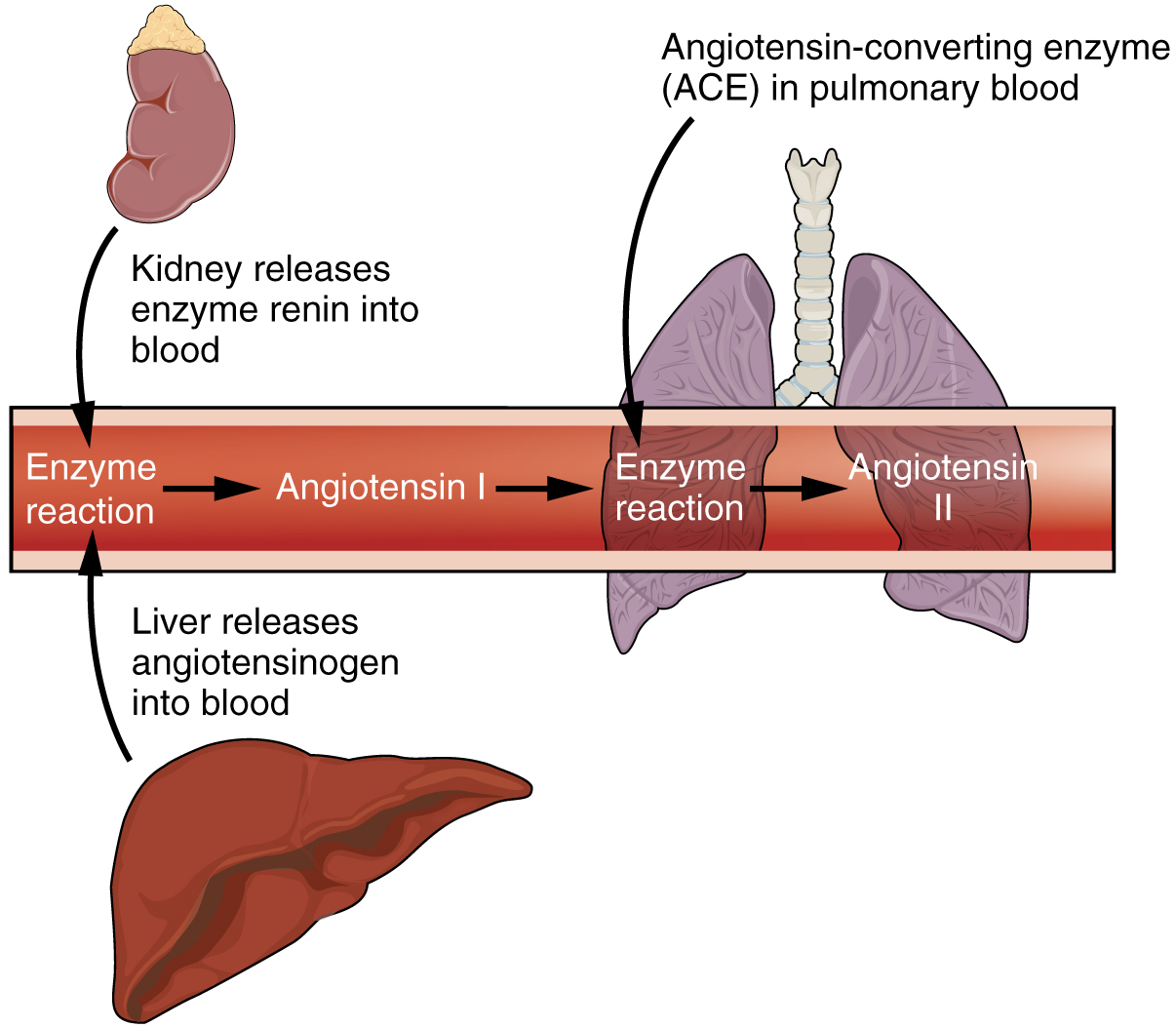
The kidneys cooperate with the lungs, liver, and adrenal cortex through the renin–angiotensin–aldosterone system (see [link] ). The liver synthesizes and secretes the inactive precursor angiotensinogen. When the blood pressure is low, the kidney synthesizes and releases renin. Renin converts angiotensinogen into angiotensin I, and ACE produced in the lung converts angiotensin I into biologically active angiotensin II ( [link] ). The immediate and short-term effect of angiotensin II is to raise blood pressure by causing widespread vasoconstriction. angiotensin II also stimulates the adrenal cortex to release the steroid hormone aldosterone, which results in renal reabsorption of Na + and its associated osmotic recovery of water. The reabsorption of Na + helps to raise and maintain blood pressure over a longer term.
Blood pressure and osmolarity are regulated in a similar fashion. Severe hypo-osmolarity can cause problems like lysis (rupture) of blood cells or widespread edema, which is due to a solute imbalance. Inadequate solute concentration (such as protein) in the plasma results in water moving toward an area of greater solute concentration, in this case, the interstitial space and cell cytoplasm. If the kidney glomeruli are damaged by an autoimmune illness, large quantities of protein may be lost in the urine. The resultant drop in serum osmolarity leads to widespread edema that, if severe, may lead to damaging or fatal brain swelling. Severe hypertonic conditions may arise with severe dehydration from lack of water intake, severe vomiting, or uncontrolled diarrhea. When the kidney is unable to recover sufficient water from the forming urine, the consequences may be severe (lethargy, confusion, muscle cramps, and finally, death) .
Sodium, calcium, and potassium must be closely regulated. The role of Na + and Ca ++ homeostasis has been discussed at length. Failure of K + regulation can have serious consequences on nerve conduction, skeletal muscle function, and most significantly, on cardiac muscle contraction and rhythm.
Recall that enzymes lose their three-dimensional conformation and, therefore, their function if the pH is too acidic or basic. This loss of conformation may be a consequence of the breaking of hydrogen bonds. Move the pH away from the optimum for a specific enzyme and you may severely hamper its function throughout the body, including hormone binding, central nervous system signaling, or myocardial contraction. Proper kidney function is essential for pH homeostasis.
Acute kidney injury can be caused by a number of factors, including transplants and other surgeries. It affects 7–10 percent of all hospitalized patients, resulting in the deaths of 35–40 percent of inpatients. In limited studies using mesenchymal stem cells, there have been fewer instances of kidney damage after surgery, the length of hospital stays has been reduced, and there have been fewer readmissions after release.
How do these stem cells work to protect or repair the kidney? Scientists are unsure at this point, but some evidence has shown that these stem cells release several growth factors in endocrine and paracrine ways. As further studies are conducted to assess the safety and effectiveness of stem cell therapy, we will move closer to a day when kidney injury is rare, and curative treatments are routine.
The effects of failure of parts of the urinary system may range from inconvenient (incontinence) to fatal (loss of filtration and many others). The kidneys catalyze the final reaction in the synthesis of active vitamin D that in turn helps regulate Ca ++ . The kidney hormone EPO stimulates erythrocyte development and promotes adequate O 2 transport. The kidneys help regulate blood pressure through Na + and water retention and loss. The kidneys work with the adrenal cortex, lungs, and liver in the renin–angiotensin–aldosterone system to regulate blood pressure. They regulate osmolarity of the blood by regulating both solutes and water. Three electrolytes are more closely regulated than others: Na + , Ca ++ , and K + . The kidneys share pH regulation with the lungs and plasma buffers, so that proteins can preserve their three-dimensional conformation and thus their function.
Bagul A, Frost JH, Drage M. Stem cells and their role in renal ischaemia reperfusion injury. Am J Nephrol [Internet]. 2013 [cited 2013 Apr 15]; 37(1):16–29. Available from: (External Link)

Notification Switch
Would you like to follow the 'Anatomy & Physiology: energy, maintenance and environmental exchange' conversation and receive update notifications?